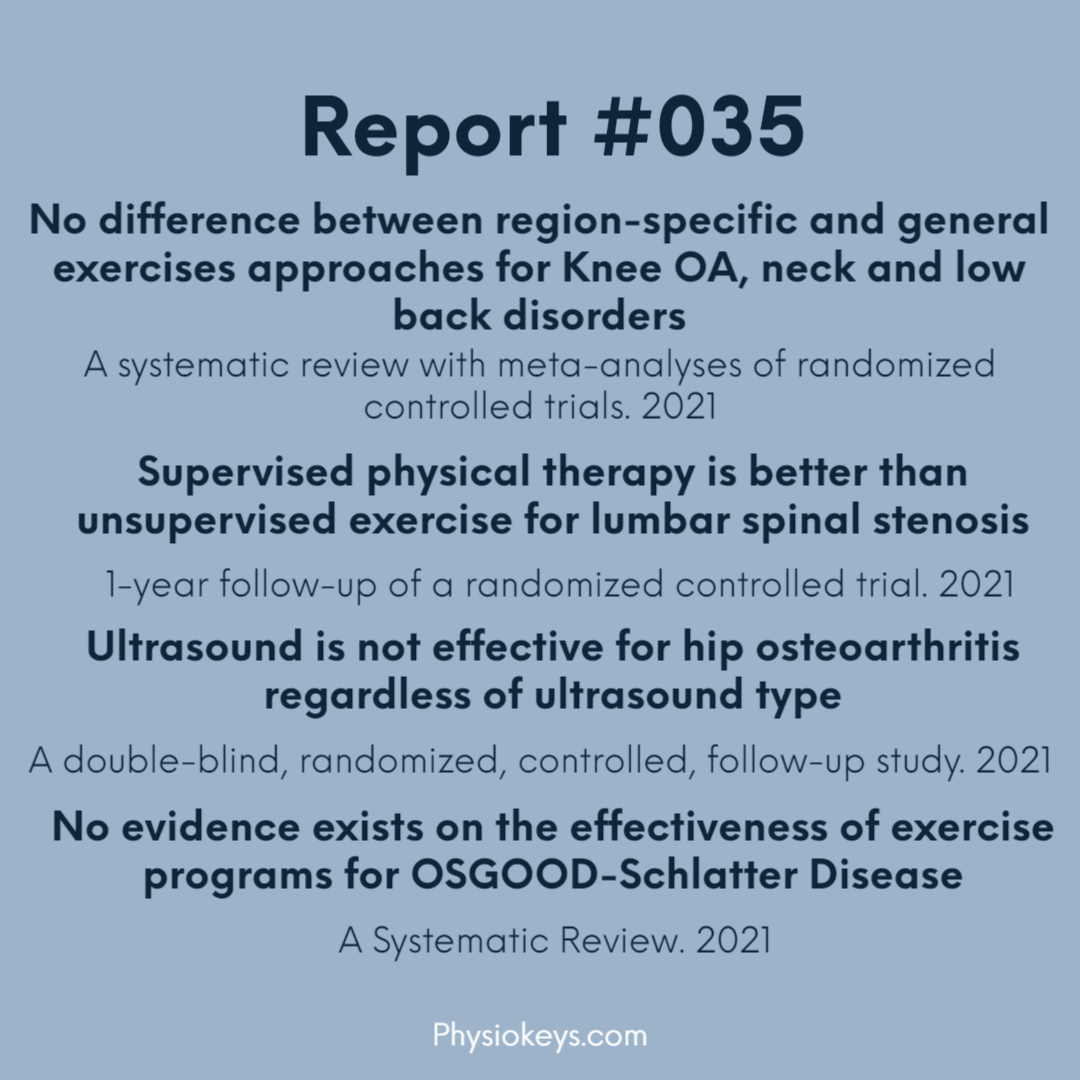
#035 – Knee OA, Hip OA, Lumbar Stenosis and OSGOOD-Schlatter Disease
Estimated reading time: 3 minutes
No difference between region-specific and general exercises approaches for Knee OA, neck and low back disorders
 Aim
Aim
- To compare the efficacy of region-specific exercises to general exercises approaches for adults with spinal or peripheral musculoskeletal disorders (MSKDs)
 Results
Results
- 18 RCRs, 313 Participant with chronic neck disorders, 1096 participant with low back disorders, 310 participant knee OA.
- No statistically significant differences between region-specific and general exercises for pain and disability reductions, based on low quality evidence in short-term, very low quality evidence in mid and long term.
 Conclusion
Conclusion
- Based on very low to low quality evidence, there appear to have no differences between both types of exercise approaches for pain reduction or disability for adults with spinal disorders.
Supervised physical therapy is better than unsupervised exercise for lumbar spinal stenosis
 Aim
Aim
- To compare the 1-year outcomes of patients with lumbar spinal stenosis treated with supervised physical therapy or unsupervised exercise.
 Interventions
Interventions
- Supervised group: supervised physical therapy sessions twice a week for 6 weeks and home exercise program.
- Unsupervised group: 6-week home exercise program only.
 Outcome measures
Outcome measures
- Zurich claudication questionnaire for symptom severity and symptom severity, SF-36 bodily pain, SF-36 general health, and the surgery rate after 1 year.
 Results
Results
- 86 participant with symptoms of neurogenic claudication caused by lumbar spinal stenosis.
- At 1 year follow-up, supervised exercise reached the minimum clinically important differences in all outcome measures.
- Surgery rate was lower for supervised group at 7% than unsupervised group at 23.3%.
 Conclusion
Conclusion
- Supervised physical therapy produced greater improvements in symptom severity and physical function than unsupervised exercise and was associated with lower likelihood of receiving surgery within 1 year.
Ultrasound is not effective for hip osteoarthritis regardless of ultrasound type
 Aim
Aim
To compare the effects of various types of ultrasound therapy (UST) on pain, function, and quality of life in patients with hip osteoarthritis.
 How
How
71 participant randomly allocated into four treatment groups:
- Continuous UST.
- Pulsed UST.
- UST combined with TENS.
- Placebo UST.
Outcome measures
Taken before, after treatments and at 3 months.
- Hip pain using Visual Analog Scale (VAS)
- Medication use
- functional impairment using Western Ontario and McMaster Universities Arthritis Index; 6-minute walking test.
- Quality of life using SF-36.
 Results
Results
- Resting pain improved significantly in all treatment groups at the follow-up compared to baseline.
- The proportion of patients achieving Minimal Clinically Important Improvement (MCII) in function at month 3 was the highest in group 3 (73%).
- The 6-minute walking test significantly improved in each group during the follow-up period.
- Pain (group1-4) and general health domains of the SF-36 showed the greatest improvement (group 2–4).
 Conclusion
Conclusion
- There was no difference among the effects of various types of UST on pain, function, and quality of life in the treatment of hip osteoarthritis.
- Additional ultrasound treatment is not likely to increase the effect of the conventional therapy on pain and function in hip osteoarthritis.
No evidence exists on the effectiveness of exercise programs for OSGOOD-Schlatter Disease
 Results
Results
- 13 studies, comprising only two RCTs, included 747 patients with 937 affected knees.
- Two randomized controlled trials exist, both investigated injection therapy.
- No evidence exists on the effectiveness of exercise programs for these adolescents.
 Conclusion
Conclusion
- Certain therapeutic approaches, such as stretching, have apparent efficacy, but no RCT comparing specific exercises with sham or usual-care treatment exists.
- Carefully controlled studies on well-described treatment approaches are needed to establish which conservative treatment options are most effective for patients with OSD.
Thank you for reading, see you in the next one.
[mailerlite_form form_id=2]